Emergency departments across the U.S. are experiencing record patient volumes, with over 130 million visits annually according to the Centers for Disease Control and Prevention (CDC). As emergency rooms grow more crowded and complex, the demand for highly skilled emergency nurse practitioners (ENPs) continues to rise. These advanced practice providers bridge the gap between nursing and medicine, offering rapid, evidence-based care to patients in critical situations.
If you’re a nurse with a passion for acute care, fast decision-making, and working under pressure, becoming an ENP may be the perfect next step in your career. This guide outlines every step—from your initial nursing education through national certification—and offers in-depth, actionable insights to support your journey. Whether you are exploring this path for the first time or are already in practice and seeking to specialize, this comprehensive roadmap will help you move forward with confidence.
You will learn how to select the right academic program, prepare for emergency-specific certification, and maintain your credentials over time. You’ll also gain a realistic view of ENP salaries, job prospects, and day-to-day responsibilities. Each section builds on the last to help you structure a successful, rewarding career in emergency care.
What Is an Emergency Nurse Practitioner?
Emergency nurse practitioners are advanced practice registered nurses (APRNs) who receive specialized education and training in emergency medicine. They often serve as front-line providers in high-acuity settings such as emergency departments, trauma units, and urgent care centers.
These professionals are qualified to assess, diagnose, and treat acute injuries and illnesses. They interpret diagnostic imaging and lab tests, perform advanced procedures like intubation or central line placement, prescribe medications, and make quick clinical decisions that may save lives. Their ability to work independently, especially in rural or underserved areas, expands access to urgent care.
ENPs are an essential part of the care team, often working collaboratively with physicians, nurses, specialists, and support staff. To understand how this role compares with others in the field, explore nurse practitioner roles and specializations for a broader perspective on advanced nursing opportunities.
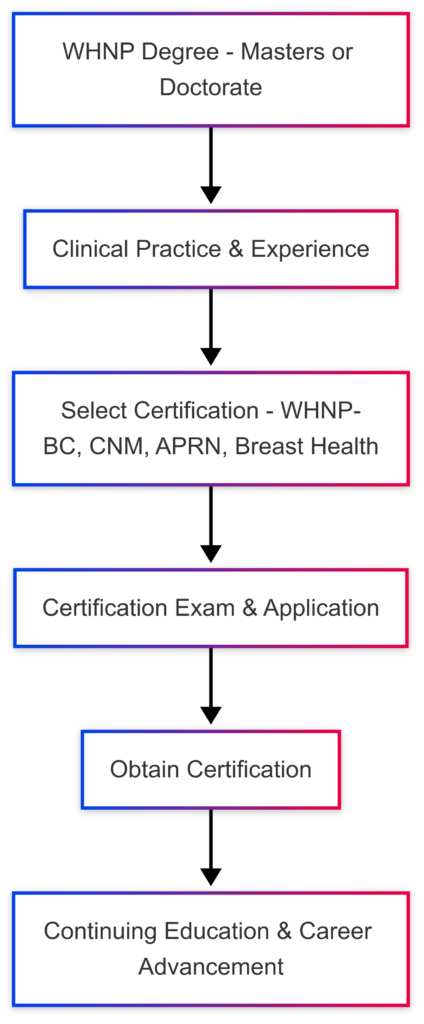
Steps to Become an Emergency Nurse Practitioner
Each step in the ENP career path builds essential knowledge, skills, and credentials. Below is an expanded look at the journey from RN licensure to ENP board certification, including educational options, real-world experience, and certification milestones.
Step 1: Earn a Bachelor of Science in Nursing (BSN)
A BSN lays the groundwork for a future in emergency nursing. This undergraduate degree covers topics such as health assessment, evidence-based practice, patient safety, and leadership in nursing. It also includes clinical rotations across multiple specialties, including potential experience in emergency or acute care settings.
You can choose between traditional four-year BSN programs or accelerated BSN pathways if you already hold a degree in another field. If you’re currently an RN with an associate degree, RN-to-BSN bridge programs are also available. For guidance on programs, check out online BSN programs for aspiring nurse practitioners.
Real-World Tip: Gaining exposure to emergency care early—such as shadowing or volunteering in an ER—can solidify your interest and inform future academic and clinical choices.
Step 2: Become a Licensed Registered Nurse (RN)
After completing a BSN program, the next step is passing the NCLEX-RN exam to become licensed. The license allows you to begin clinical practice, which is essential for building the skills needed in high-pressure, fast-paced emergency environments.
To prepare for the NCLEX, many students take practice exams and join study groups. For official exam information and resources, visit the National Council of State Boards of Nursing (NCSBN).
Insight: During your early years of practice, seek employment in hospitals or healthcare systems with high ER volumes. This will enhance your learning curve and allow you to apply foundational skills in real-world scenarios.
Step 3: Gain Experience in Emergency Nursing
Before applying to a graduate program with a focus on emergency care, hands-on experience is invaluable. Most nurse practitioner programs require or prefer at least 1-2 years of experience in an emergency department or similar acute care setting. These roles provide the clinical judgment and confidence required for more autonomous practice as an ENP.
Case Example: One nurse worked two years in a high-volume trauma center and used that experience to apply for an ENP post-master's program. Her background allowed her to excel during her practicum placements and eventually secure a role at a Level I trauma center.
Step 4: Complete a Graduate Nurse Practitioner Program
To become an ENP, you must complete either a Master of Science in Nursing (MSN) or Doctor of Nursing Practice (DNP) degree. While most ENPs begin as Family Nurse Practitioners (FNPs), others may follow an Acute Care Nurse Practitioner (ACNP) path and pursue additional emergency-focused training.
Choose a program accredited by the Commission on Collegiate Nursing Education (CCNE) or the Accreditation Commission for Education in Nursing (ACEN).
Program Comparison Table:
| Program Type | Typical Duration | Common Formats | Specialty Focus |
| MSN-FNP | 2-3 years | Online, Hybrid | Primary Care |
| DNP | 3-4 years | Hybrid, On-Campus | Advanced Clinical, Leadership |
| Post-Master's Certificate | 1-1.5 years | Online | Emergency Specialty |
Pro Tip: Look for programs that offer emergency-focused clinical practicums or residencies. Some universities have formal ENP concentrations, while others partner with hospitals to provide immersive ER training experiences.
Step 5: Obtain Nurse Practitioner Certification
After earning your graduate degree, the next step is certification. Most ENPs certify as Family Nurse Practitioners before pursuing additional emergency credentials. Certification validates your competence in providing independent, comprehensive care across the lifespan.
National certifying bodies include:
- American Nurses Credentialing Center (ANCC)
- American Academy of Nurse Practitioners Certification Board (AANPCB)
Many employers require this certification for initial licensure and employment. It is also a prerequisite for emergency-specific credentials.
Step 6: Earn Emergency Nurse Practitioner Certification
The Emergency Nurse Practitioner Certification (ENP-C), offered by the AANPCB, is the recognized credential for FNPs who wish to validate their expertise in emergency care. The ENP-C signifies proficiency in high-acuity, fast-paced environments.
Eligibility Criteria Include:
- Current RN license in good standing
- National certification as an FNP (FNP-C or FNP-BC)
- Completion of an emergency-focused academic program or a minimum of 2,000 hours of emergency clinical practice
ENP Exam Topics:
- Acute and trauma care
- Pharmacologic interventions
- Emergency diagnostic testing
- Evidence-based emergency protocols
Study Tip: ENP exam prep materials are available through professional organizations and may include practice exams, webinars, and review courses.
Step 7: Obtain State Licensure and Practice Authority
State licensure is the final step before practicing as an ENP. While national certification demonstrates competency, each state sets its own rules regarding scope of practice, prescriptive authority, and supervision requirements.
Consult the AANP state practice environment guide for detailed licensing information. Full-practice states allow NPs to diagnose and prescribe independently, while others require physician collaboration.
Actionable Insight: Apply for DEA registration if you plan to prescribe controlled substances. This process can take several weeks and often requires proof of state licensure.
Continuing Education and Credential Maintenance
Once certified and licensed, ENPs must maintain their credentials through continuing education. Requirements typically include:
- 100 CE hours every five years for AANPCB recertification
- Renewals of ACLS, PALS, and trauma certifications like TNCC
- Completion of any state-mandated courses such as pain management or pharmacology
Professional Development Tip: Membership in the Emergency Nurses Association (ENA) or American Association of Nurse Practitioners (AANP) provides access to discounted CE, networking opportunities, and clinical resources.
Salary and Job Outlook for Emergency Nurse Practitioners
The job outlook for ENPs is highly favorable. The U.S. Bureau of Labor Statistics projects a 38% increase in NP employment from 2022 to 2032, driven by expanded healthcare access and demand for urgent care services.
For additional career insights, view data on the highest-paying nurse practitioner specialties.
ENP Salary Breakdown:
| Experience Level | Annual Salary Range |
| Entry-Level | $110,000 – $120,000 |
| Mid-Career | $125,000 – $135,000 |
| Experienced | $140,000 – $150,000+ |
Geographic location, facility type, and hours worked also influence salary. ENPs working nights, weekends, or in underserved areas often earn bonuses or stipends.
Why Become an Emergency Nurse Practitioner?
The role of ENP is uniquely challenging and rewarding. These clinicians function at the intersection of nursing compassion and medical precision, providing high-quality care in moments of crisis. From managing trauma cases to rapidly stabilizing critically ill patients, ENPs are trusted leaders in emergency settings.
Career Benefits:
- Significant autonomy and responsibility
- Procedural skill development (e.g., suturing, intubation)
- High salary potential
- Daily variety and impact
Take the Next Step Toward Emergency Practice
The journey to becoming an emergency nurse practitioner demands focus, determination, and a passion for acute care. By building strong clinical foundations, pursuing advanced education, and securing board certification, you can unlock a career filled with purpose, respect, and leadership.
To get started, explore online nurse practitioner programs aligned with emergency care, reach out to current ENPs for mentorship, and map out your path to certification and licensure. Every shift in the ER offers the chance to make a life-saving difference—and it all begins with the right training.
Sources
- Centers for Disease Control and Prevention (CDC)
- National Council of State Boards of Nursing (NCSBN)
- Commission on Collegiate Nursing Education (CCNE)
- Accreditation Commission for Education in Nursing (ACEN)
- American Nurses Credentialing Center (ANCC)
- American Academy of Nurse Practitioners Certification Board (AANPCB)
- Emergency Nurses Association (ENA)
- American Association of Nurse Practitioners (AANP)
- U.S. Bureau of Labor Statistics (BLS)